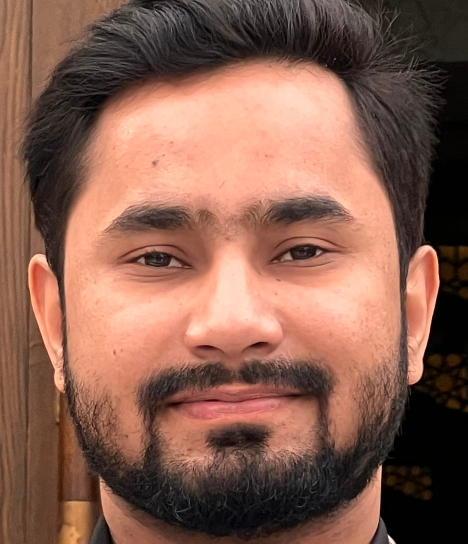
概要
To obtain a challenging position at an organization that will allow me to put my skills, experience, and education to the best possible use.
工作经历
Credentialing Analyst and Consultant
I've been working as a Credentialing Analyst and Consultant at MD Tech, Job Responsibilities are mentioned below;
New practice setup in all 50 states.
Complete data verification with insurances including effective date, provider id and plans etc.
Credentialing of Behavioral Health, Dental, Medical, Telehealth, Multispecialty Group, Pharmacy, Lab, Urgent Care Centers, IDTF and CORF.
Credentialing of all mid-levels (PA, NP, ARNP) and MD's.
Adding additional providers to a current practice.
Obtain NPI Type 1 and Type 2.
Re-attestation of CAQH Proview and document maintenance.
I&A, NPPES, PECOS, Availity, CAQH Enrollhub and PaySpan accounts creation & maintenance.
Re-validation/Re-credentialing of all payors.
EDI, ERA, EFT and Clearing House Setup.
Demographic changes/updates.
Contract Re-Negotiation.
Personalize provider representatives of each insurance with contact details for any concern.
Regular and strong follow up with insurance carriers.
Maintaining Credentialing Grid with participating status.
Provider Licensing and Renewals in all 50 states of US.
Understanding/compliance of HIPAA laws and regulations.
Computer proficiency (MS Office – Word, Excel and Outlook).
Able to prioritize and adapt.
Don't let credentialing difficulties affect your revenue any longer, So allow me to take care of your payor relationships.
Credentialing and Enrollment Executive
I worked as a Credentialing & Enrollment Executive for P3 Healthcare Solutions, where I was responsible for enrolling providers in Medicare, Medicaid, and Commercial payers, as well as data verification, form filling, follow-up on credentialing applications, document maintenance and making credentialing grid.